Persistent Hyperbilirubinemia and Marked Transaminase Elevation After 10 Days of Treatment

Homeopathic Management of Elevated Glycohemoglobin (HbA1c)
November 23, 2025Case Study: Persistent Hyperbilirubinemia and Marked Transaminase Elevation After 10 Days of Treatment
Patient Profile
-
Name: Subhan Husnain
-
Age: 9 years
-
Date of Report: 09 November 2025
-
Setting: AlKhidmat Raazi Diagnostics, Rawalpindi
-
Department: Outdoor / Chemical Pathology
Background
This case involves a paediatric patient undergoing evaluation for liver dysfunction after 10 days of ongoing treatment for a suspected hepatic condition. The patient was initially diagnosed with jaundice and elevated liver enzymes. Over the course of management, serial liver function tests were advised to monitor improvement or deterioration.
Ten days into treatment, follow-up laboratory investigations revealed persistent hyperbilirubinemia and markedly elevated alanine transaminase (ALT). These findings prompted a reassessment of the underlying cause, disease progression, and the effectiveness of ongoing therapy.
Clinical Presentation
The patient reportedly presented with:
-
Yellow discoloration of the eyes and skin (jaundice)
-
Reduced appetite
-
Mild fatigue
-
Dark-coloured urine
-
No significant bleeding tendencies reported
-
No history suggestive of chronic liver disease
No detailed initial laboratory values were provided, but the current follow-up report indicates that enzyme levels remain considerably elevated.
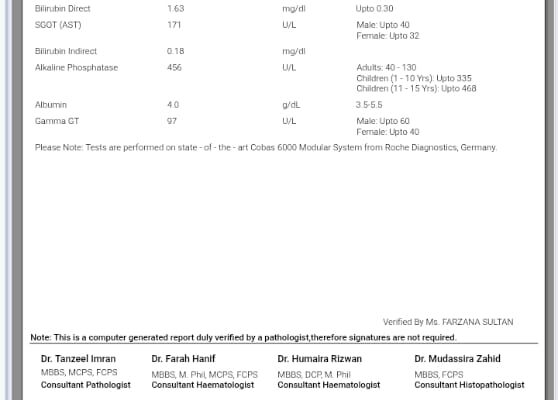
Laboratory Findings (09 November 2025)
| Test | Result | Reference Range |
|---|---|---|
| Total Bilirubin | 5.63 mg/dL | 0.1–1.2 |
| Direct Bilirubin | 5.28 mg/dL | ≤0.30 |
| Indirect Bilirubin | 0.35 mg/dL | — |
| ALT (SGPT) | 1092 U/L | Male ≤41 |
| AST (SGOT) | 482 U/L | Male ≤40 |
| Alkaline Phosphatase | 710 U/L | 40–130 (Adults), 1–10 yrs ≤335; 11–15 yrs ≤468 |
| Gamma GT | 301 U/L | Male ≤60 |
| Albumin | 3.5 g/dL | 3.5–5.5 |
Interpretation of Findings
1. Persistent Direct Hyperbilirubinemia
With a direct bilirubin of 5.28 mg/dL, the pattern clearly points toward:
-
Cholestasis (impaired bile flow)
-
Hepatocellular injury affecting bilirubin excretion
The minimal elevation in indirect bilirubin confirms that haemolysis is unlikely.
2. Markedly Elevated ALT (1092 U/L)
ALT levels in the thousands typically indicate acute hepatic injury. The primary causes include:
-
Acute viral hepatitis (A, B, E)
-
Drug-induced liver injury (antibiotics, anti-TB drugs, paracetamol toxicity)
-
Autoimmune hepatitis
-
Ischemic hepatitis
Given the age of the patient, viral hepatitis or drug-induced injury are common considerations.
3. Elevated AST and GGT
-
AST at 482 U/L supports hepatocellular injury.
-
GGT at 301 U/L strongly suggests biliary involvement or cholestasis.
4. Alkaline Phosphatase (ALP) Elevated at 710 U/L
A raised ALP, especially in combination with high direct bilirubin and GGT, reinforces the suspicion of:
-
Obstructive liver disease
-
Hepatitis-related cholestatic phase
-
Drug-induced cholestasis
5. Albumin at Lower Normal Limit (3.5 g/dL)
Albumin remains acceptable, indicating preserved synthetic liver function. This is reassuring and suggests the condition is acute rather than chronic.
Clinical Assessment
The laboratory parameters indicate ongoing hepatocellular damage combined with a cholestatic component. The persistently high ALT after 10 days suggests:
-
Partial improvement (if previous values were higher), or
-
Inadequate response to therapy (if previous values were lower)
The dominance of direct bilirubin and raised cholestatic enzymes indicates impaired bile excretion, which can prolong jaundice despite treatment.
Possible Differential Diagnoses
-
Acute Viral Hepatitis (HAV or HEV common in children in Pakistan)
-
Drug-Induced Liver Injury (DILI)
-
Autoimmune Hepatitis
-
Obstructive Pathology (bile duct obstruction, though less likely without severe symptoms)
-
Metabolic or Genetic Liver Disorders (less likely given acute onset)
Management Considerations
-
Continuation of Supportive Care
Adequate hydration, nutrition, and avoidance of hepatotoxic medications. -
Repeat LFTs Every 3–5 Days
Monitoring the downward trend of ALT and bilirubin is essential. -
Ultrasound Abdomen
To rule out structural or obstructive causes. -
Viral Serology
HAV IgM, HEV IgM, HBsAg, Anti-HCV recommended. -
Medication Review
Identification and discontinuation of any hepatotoxic drugs. -
If no improvement:
Consider referral to a paediatric hepatologist.
Conclusion
This case highlights a child with ongoing liver inflammation 10 days after treatment initiation, as evidenced by elevated ALT (1092 U/L), high direct bilirubin (5.28 mg/dL), and raised cholestatic enzymes. While synthetic liver function remains intact, the biochemical pattern suggests significant acute hepatocellular injury likely due to viral or drug-induced causes. Close monitoring, repeat investigations, and targeted evaluation for hepatitis or cholestasis are essential for appropriate management and recovery.